Dr. Marco V. Benavides Sánchez. Medmultilingua.com /
In medicine, major breakthroughs rarely arrive overnight. More often, they emerge quietly as supportive tools that gradually reshape how decisions are made. Artificial intelligence (AI) fits firmly into this category. It does not replace clinicians, but it is beginning to transform one of the most complex areas of modern medicine: organ transplantation.
Today, when a scarce organ must be allocated within hours and every variable matters, AI offers something essential: the ability to integrate information that was previously assessed in isolation. Clinical records, laboratory results, medical imaging, genetic markers and patient history can now be analysed together, producing a more comprehensive — and potentially fairer — picture.
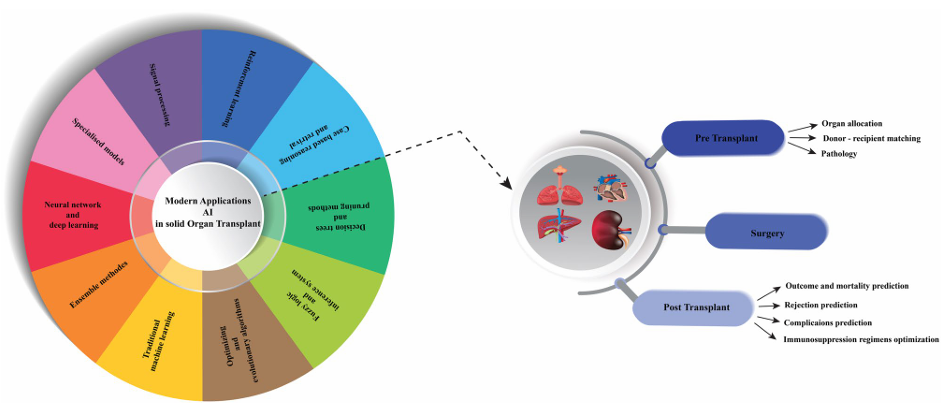
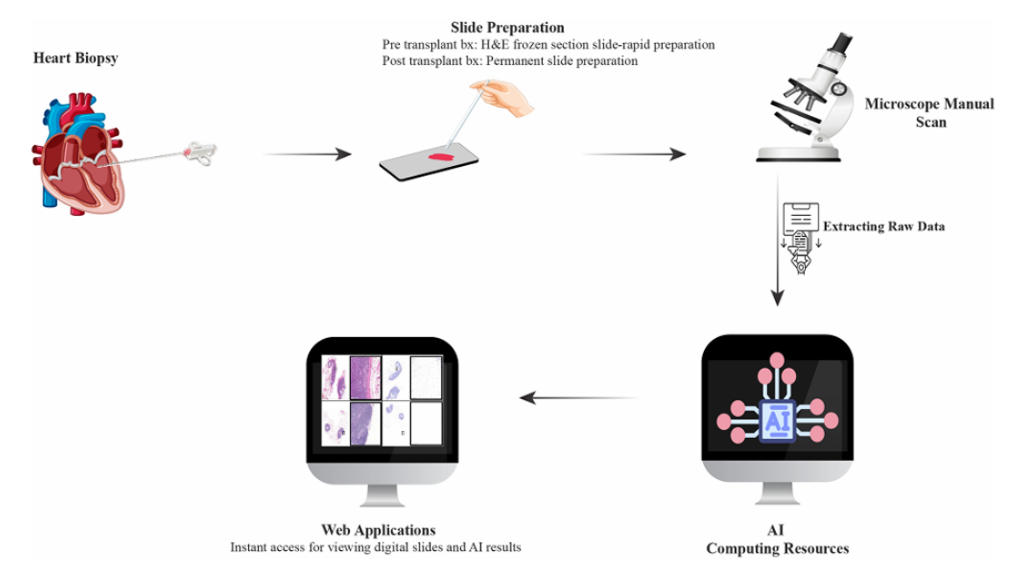
This evolving approach is explored in a recent scientific review published in the Journal of Translational Medicine. The paper shows how AI is already influencing every stage of the transplant pathway, from pre‑transplant assessment to long‑term follow‑up after surgery.
By: Arjmandmazidi et al. Journal of Translational Medicine
(2025) 23:678
Before transplantation: when getting it right matters as much as acting quickly
A transplant waiting list is not simply a queue. It is a highly complex system where medical urgency, biological compatibility and realistic chances of success intersect. For decades, these decisions have relied on well‑established guidelines and clinical experience. AI does not replace this expertise, but it adds an additional analytical layer.
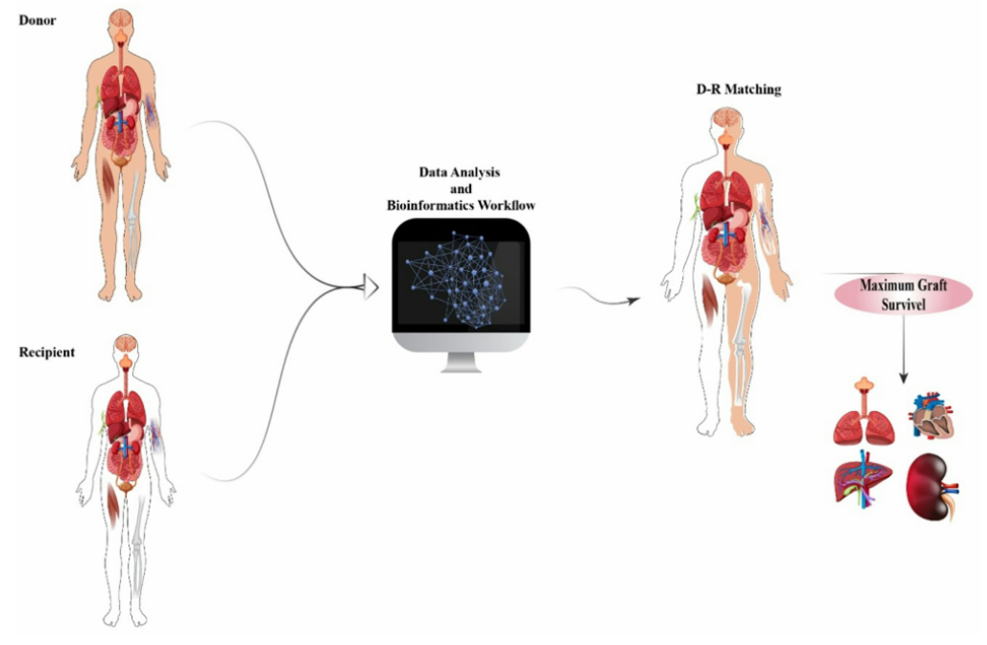
Using machine‑learning algorithms, AI systems can review thousands of previous transplant cases and identify patterns associated with better outcomes. This helps refine donor–recipient matching and reduces the risk of early rejection or graft failure.
From a translational medicine perspective, the true value of AI lies in its ability to turn vast amounts of data into clinically meaningful insights. The goal is not automated decision‑making, but clearer, evidence‑informed scenarios that support clinicians in making the best possible choices.

By: Arjmandmazidi et al. Journal of Translational Medicine
(2025) 23:678
In the operating theatre: technology that supports, not supplants
During transplant surgery, the surgeon remains central. However, technology is increasingly playing a supportive role. In some centres, AI is integrated into robot‑assisted surgical systems, offering greater precision and stability during particularly delicate procedures.
Arjmandmazidi et al. Journal of Translational Medicine
(2025) 23:678
Real‑time image analysis, identification of critical anatomical structures and optimisation of surgical movements illustrate how AI can help reduce risk without shifting responsibility away from the clinical team. The message is clear: the technology does not operate independently — it works alongside human judgement.
After transplantation: anticipating rather than reacting
The success of a transplant does not end in the operating theatre. The real challenge begins afterwards, when the patient’s body must accept a foreign organ while adapting to lifelong immunosuppressive therapy.
At this stage, AI offers a key advantage: anticipation. By analysing laboratory trends, demographic factors and genetic profiles, algorithms can estimate the risk of rejection, infection or other complications before they become clinically apparent.
Another important development is the ability to predict how individual patients will absorb and metabolise medications after transplantation. More personalised dosing can improve treatment effectiveness while minimising side effects — a central aim of precision medicine.
By: Arjmandmazidi et al. Journal of Translational Medicine
(2025) 23:678
What does this mean for patients?
From the patient’s perspective, the introduction of AI does not signal a move towards impersonal medicine. On the contrary, better‑informed decisions can lead to improved outcomes, fewer complications and follow‑up care tailored more closely to individual needs.
AI does not deliver final verdicts. It functions as a decision‑support tool, highlighting risks, probabilities and alternative pathways. The final decision remains with the clinical team, who integrate these insights with direct patient assessment and the broader human context of each case.
By: Arjmandmazidi et al. Journal of Translational Medicine
(2025) 23:678
A quiet but profound shift
The review published in the Journal of Translational Medicine confirms a clear trend: artificial intelligence is already part of contemporary organ transplantation. Significant challenges remain, including ongoing clinical validation and equitable access to these technologies, but the direction of travel is evident.
In a field where every decision may represent a second chance at life, AI is emerging as a strategic ally. It does not replace medical expertise or the doctor–patient relationship, but it expands our ability to understand risk, anticipate problems and make better decisions. And in medicine, better decisions often make the difference between survival and truly living.
Reference
Arjmandmazidi, S., Heidari, H. R., Ghasemnejad, T., Mori, Z., Molavi, L., Meraji, A., Kaghazchi, S., Mehdizadeh Aghdam, E., & Montazersaheb, S. (2025). An in‑depth overview of artificial intelligence (AI) tool utilisation across diverse phases of organ transplantation. Journal of Translational Medicine, 23(1), 678. https://doi.org/10.1186/s12967-025-06488-1
#ArtificialIntelligence #Medicine #Surgery #Medmultilingua


Leave a Reply